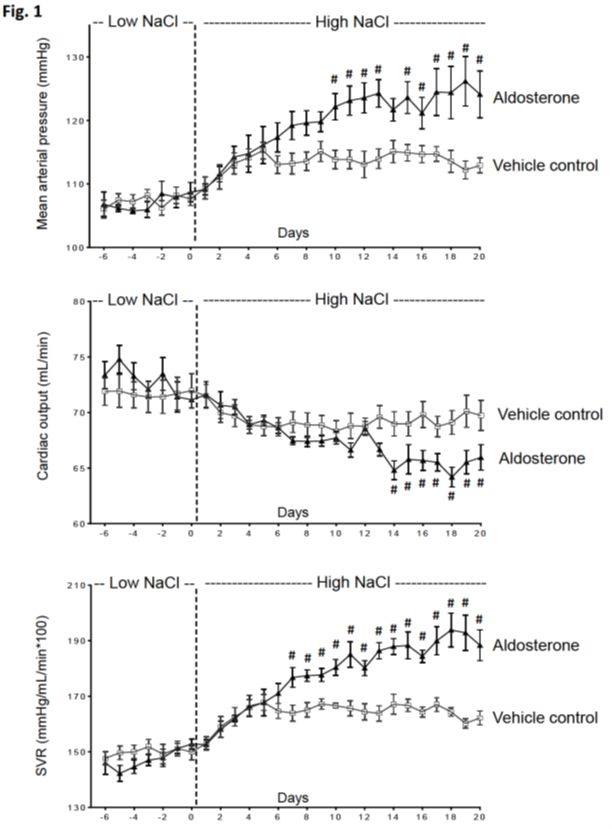
Primary aldosteronism is the most common form of secondary hypertension, accounting for up to 50% of hypertension induced by excess salt intake. According to the traditional volume loading theory, hyperaldosteronism in salt-sensitive individuals is thought to induce sodium and water retention, resulting in a rise in blood volume and subsequent increase in cardiac output initiating hypertension. Systemic vascular resistance is thought to increase only as a secondary consequence of increased cardiac output and blood pressure through so-called autoregulation. However, a growing body of evidence suggests that aldosterone may influence blood pressure not only through its effects on the kidney, but through direct effects on vascular tone (vascular resistance). Therefore, we investigated the primary hemodynamic mechanism by which hyperaldosteronism promotes salt sensitivity and the initiation of salt-dependent hypertension in Sprague Dawley rats given an infusion of aldosterone (model of primary aldosteronism) or vehicle (control group). Using implanted arterial pressure telemetry probes and Doppler ultrasound flow probes, we continuously monitored changes in mean arterial pressure, cardiac output, and systemic vascular resistance in response to increases in salt intake. In aldesterone-infused rats, compared with control rats, there was a significantly greater increase in blood pressure and systemic vascular resistance and a concomitant significant decrease in heart rate and cardiac output when switching from a low-salt to a high-salt diet (Figure). These results provide evidence that aldosterone promotes salt sensitivity and the initiation of salt-dependent hypertension by inducing an increase in systemic vascular resistance after salt intake while decreasing cardiac output. Thus, an increase in cardiac output is not necessary for the initiation or maintenance of hypertension. These findings challenge the traditional volume loading theory and instead support the vasodysfunction theory, which posits an increase in systemic vascular resistance as the primary cause of hypertension initiation (Kurtz et al., 2023).
Mean arterial pressure (MAP), cardiac output (CO), and systemic vascular resistance (SVR) (24-h averages) during administration of a low-salt diet (0.26% NaCl) and a high-salt diet (4% NaCl) in vehicle-infused control rats and aldosterone-infused rats. The # symbol indicates p < 0.05.